 RSS FEED
RSS FEED
Posts Tagged ‘Migraine treatment’
Botox for Head Implosion, not Explosion?
February 17th, 2010
A new study of 18 Migraine sufferers reported in the Archives of Dermatology Monday indicates that Botox may be helpful for those who describe their pain as “crushing” or “eye-popping.” That’s an interesting new  distinction. So, not so good for those of us, like me, who walk around saying “My head explode!”
distinction. So, not so good for those of us, like me, who walk around saying “My head explode!”
It’s hard to say how significant a study of 18 patients is, and previous reports on Botox for Migraines have been mixed at best. This study reports an average reduction from 7 Migraines per month to 1 Migraine per month, among those who responded to the Botox. You can read a bit more about the study here: Does Botox Stop Some Migraines? in the Minneapolis – St. Paul Star Tribune. What really interests me, though, is the fact that the description of the pain itself is indicative of whether the Botox will help or not. Pain is so subjective, and so difficult to measure, it’s fascinating that there could be a correlation between how we experience the pain and the mechanics of our Migraines.
I’m imagining a time when you can describe your pain, and get a specific treatment for it. Head imploding? Try this. Head exploding? Try that. What about that one where little people with grapefruit spoons are trying to scrape your brain off the inside of your skull? I hate that one.
– Megan
Tags: Botox, migraine, Migraine treatment, pain
Posted in Current Affairs, Medicine, Musings | Comments (5)
Migraines and Emotional Health
June 1st, 2009
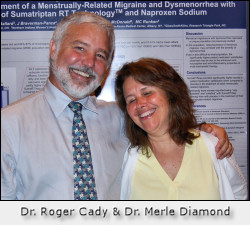 We had a very exciting teleconference yesterday with Dr. Roger Cady of the Headache Care Center of Springfield, Missori. I think everyone who was on the call will attest to what a warm and caring soul Dr. Cady is and how he puts everyone at ease. It was an upbeat call and I think everyone on the conference came away with some practical ideas they can put into use.
We had a very exciting teleconference yesterday with Dr. Roger Cady of the Headache Care Center of Springfield, Missori. I think everyone who was on the call will attest to what a warm and caring soul Dr. Cady is and how he puts everyone at ease. It was an upbeat call and I think everyone on the conference came away with some practical ideas they can put into use.
We discussed the extra sensitivity of a Migrainous nervous system and how to care for that nervous system – not as something wrong or diseased, but as a process of acceptance of who we are, of the unique person we are. When we are blessed with that extra level of sensitivity, we are sensitive to emotional cues and issues as well. Anxiety and depression are described as “co-morbid” with Migraine because they occur together but the causal relationship is not understood at this time. The connection is probably in serotonin which is implicated in Migraine and in anxiety and depression.
If you’d like to listen to the audio of the teleconference and you are already registered for the Managing Life with Migraine teleconferences, sit tight. We will have the audio file posted within the week and will email you the link. If you aren’t yet registered, please go to Managing Life with Migraine and get on the list! This will give you access to all the teleconference recordings as well as a spot on future teleconferences. Next month’s call on Sunday, June 28th will be with Dr. William Young of the Jefferson Headache Center.
– Megan Oltman
Photo of Dr. Cady and Dr. Diamond copyright Teri Robert, used by permission.
Tags: emotional health, Migraine care, Migraine treatment
Posted in Managing, Medicine | Comments (1)
Getting the Support you Need
May 8th, 2009
 If there’s anything that makes me want to throw up my hands and give up, it’s how complex Migraine disease is. Migraine disease has multiple triggers, can take multiple forms with different symptoms and effects on our lives, and has multiple treatment possibilities. I could not manage all of this without support. It’s lonely dealing with a disease that eats away days and weeks of our lives, and isolates us where the sound and the light won’t bother us. Treating Migraine takes managing multiple aspects of our lives and health – that takes support. The people who support me remind me that every day will not be so bad, that life is still worth living, that there is hope. The things that support me give a structure to my life that I can count on when I am not functioning at my best.
If there’s anything that makes me want to throw up my hands and give up, it’s how complex Migraine disease is. Migraine disease has multiple triggers, can take multiple forms with different symptoms and effects on our lives, and has multiple treatment possibilities. I could not manage all of this without support. It’s lonely dealing with a disease that eats away days and weeks of our lives, and isolates us where the sound and the light won’t bother us. Treating Migraine takes managing multiple aspects of our lives and health – that takes support. The people who support me remind me that every day will not be so bad, that life is still worth living, that there is hope. The things that support me give a structure to my life that I can count on when I am not functioning at my best.
We need to cultivate our support systems – building them up when we feel well so they will be there when we need them. We need to do what we can for the people who support us, when we can. In other words, we need to build our stock of resources.
What kinds of support are there? Consider these:
- Professional support – this includes:
- Doctors – you need a good medical doctor to track and coordinate your care and help you find appropriate medication.
- Complementary practitioners – chiropractors, massage therapists, acupuncturists, bio-feedback practitioners, and nutritionists, among others, can help you relax, rechannel your energy, maintain your general health, manage and reduce pain.
- Therapists – migraine is not a psychological disorder! But supportive therapy can help us deal with the emotions our illness causes.
- Coaches – a coach can help you create a plan to manage your life with Migraine and help you generate the energy and enthusiasm to move ahead with your plan. That’s what I do – contact me to hear more about it. Both coaches and therapists can be a great help in picking you up when you are down.
- Personal Support:
- Friends, family members, neighbors, even bosses or co-workers. You will need to make sure that they have some basic information about Migraine and that they know you have a disease. You’ll need to be clear about what kind of support or help you need from them.
- Another great form of personal support comes from other migraineurs, whether you join an online community or group such as my personal favorite, the forum at My Migraine Connection; chat with other Migraineurs on Twitter; join or start a face to face Migraine support group; or get on the phone with other Migraineurs in a relaxation teleclass; or join one of our Managing Life with Migraine teleconferences.
- Medication support – you need medication choices to support you in preventing migraines and stopping them when they occur.
- Tool-kit support – Whatever you use to comfort yourself when you do get a migraine – comfy pillows or blankets, ice packs, hot baths, cups of tea, essential oils, soft music, soft lights, whatever you use to help you to feel better.
- Structure & routine support – this is what you do regularly to make the most of your well time and stay as well as you can. It will include your medications and nutrition, your exercise routine, relaxation routine, sleep routine.
Where is support missing in your life? Sometimes making a list of the pieces that are missing and taking just one step at a time can make a big difference. Like finding one person to talk to, or scheduling one doctor’s appointment. Giving a teleclass a try, or stocking up on comfort supplies.
What can you do to build your support system?
– Megan
Hands together image courtesy of Maria Angelie.
Tags: managing life with migraine, migraine support, Migraine treatment, migraine treatment plan
Posted in Managing, Medicine, Tips & Techniques | Comments (4)
Please Email Congress Today – The Window is Closing
March 26th, 2009
 There are two days left to get your email in to Congress (that is, today and tomorrow) requesting that they sign off on language that directs the National Institutes of Health to fully fund research on Migraine and Headache disorders. You don’t even have to think up your own email, or find your Representative’s contact information (or know who your Representative is) – all you have to do is click here for the Alliance for Headache Disorders Advocacy’s action page. There you can send your email in less than three minutes and a few clicks. If you haven’t done it already, please do it now. It will mean better treatment options for all of us. It will mean more understanding of our disease, and more options in our future. And if we don’t get enough signatures now, it will mean another year of delay, without basic research being done. Please take a few minutes out to help. I took three days out to go to D.C. on this effort. You can take three minutes without leaving your chair. Thanks!
There are two days left to get your email in to Congress (that is, today and tomorrow) requesting that they sign off on language that directs the National Institutes of Health to fully fund research on Migraine and Headache disorders. You don’t even have to think up your own email, or find your Representative’s contact information (or know who your Representative is) – all you have to do is click here for the Alliance for Headache Disorders Advocacy’s action page. There you can send your email in less than three minutes and a few clicks. If you haven’t done it already, please do it now. It will mean better treatment options for all of us. It will mean more understanding of our disease, and more options in our future. And if we don’t get enough signatures now, it will mean another year of delay, without basic research being done. Please take a few minutes out to help. I took three days out to go to D.C. on this effort. You can take three minutes without leaving your chair. Thanks!
– Megan
Cats in the window image courtesy of Helene Jutras.
Tags: Alliance for Headache Disorders Advocacy, Congress, Migraine treatment, National Institutes of Health
Posted in Advocacy | Comments (2)
Testing for Medication Allergies
October 13th, 2008

Long story ahead. I’ve been trying to get tested to get more information about the specifics of my medication allergies. I’m allergic to ibuprofen, likely all aspirin derivatives (NSAIDs) and possibly also acetominophen. Long story which you may have read here, 2 near-death anaphylactic reactions to Advil, hives from Tylenol, swollen lips from an aspirin-based product, yada-yada.
My allergist suggested at the time (nearly 6 years ago) that since all these reactions happened within a few months, when my system calmed down I might not be allergic to everything. But said allergist would not do challenge tests on me for the medications for fear of liability, and she was also a screaming nasty unprofessional person whose sorry butt got fired.
Lo, 5+ years of living without these meds later, my headache specialist would like me to get tested for aspirin and acetominophen to see if we can expand my available Migraine medication options. My primary doctor told me 6 months ago that he thought he could do such a test in his office. The idea would be that I would actually ingest a small controlled amount of the drug in question and the staff would stand by to save me if I started going into anaphylaxis. Sounds like fun, no?
So last week I went to talk to my primary doctor about doing said challenge tests in his office. He
 discussed it with me in more detail. He wanted to find a less dangerous way and proposed testing my blood for antibodies to the chemicals involved. This indicates whether there is a sensitivity, but I asked him, “Does having a sensitivity tell you whether the body would react anaphylactically?” He went off to research it and concluded that no, it wouldn’t. I just got
discussed it with me in more detail. He wanted to find a less dangerous way and proposed testing my blood for antibodies to the chemicals involved. This indicates whether there is a sensitivity, but I asked him, “Does having a sensitivity tell you whether the body would react anaphylactically?” He went off to research it and concluded that no, it wouldn’t. I just got
a call back from his nurse saying there was no way to test except the “old-fashioned” challenge test, and they felt that could only be done in the hospital with a crash cart. So I should find an allergist who would admit me as an inpatient and do the test in the hospital.
Is this back to square one? I’m imagining calling allergists’ offices and saying, “hi, I’m looking to make an appointment see if the doctor would be willing to put me in the hospital, give me something that might kill me and then stand by to save my life! Oh and by the way, I really am counting on my life being saved! Want to take me on as a patient?” The fact that I am about to switch insurance makes this all more complicated.
I’m actually going to call Dr. G (headache specialist) and see if he might think
an allergist associated with his hospital would do it. At least then it would be one doctor asking it of another instead of some crazy-sounding patient?
I’m not particularly upset here or anything, just kind of rolling my eyes. Nothing’s ever simple, is it? It’s a wonder any of us ever have time to do anything other than wade our way through our medical issues!
– Megan Oltman
Still living aspirin-free!
Aspirin image courtesy of Ritcharnd Moskow; magic pill image courtesy of [O*] ‘BharaT; map-maze image courtesy of David Bleasdale.
Tags: allergy challenge test, aspirin, headache specialists, ibuprofen, medication allergies, Migraine treatment, NSAIDs
Posted in Medicine, Rant | Comments (3)
Between a Rock and a Hard Place – How do We Choose?
September 19th, 2008
The first in a series of posts on Migraineurs making choices for our health care and our lives.
How do we choose? We are faced with choices on a daily basis. We lose sleep over them; they feel momentous, life-changing. Rarely are they an Indiana Jones moment:
- if I step on the wrong step it will crumble below me and hurl me into the rat/snake/cockroach infested pit, or
- if I stake all on drinking from the gold cup my eyeballs will melt and I will desiccate into a human husk, so that the 2000 year-old crusader can say “he chose unwisely.”
Most of our choices change our lives more gradually!
For those of us with Migraine disease and chronic illness, choices often revolve around
- what treatments to try, and
- how to manage to make our living.
Most choices in life are reversible; we can change our minds, have a chance to learn from our mistakes. Usually there is no one clear right choice. In medical situations we often wish there was one. How about the doctor coming to us and saying, “Well, Ms. So and So, here’s the choice
1. If you take this course of treatment it will cost you $2500 and you will feel worse for 2 months, 3 days and 16 hours, but then you will lose 30 pounds, become a natural blond, your Migraines will cease  forever and you will never age another day.
forever and you will never age another day.
2. On the other hand if you don’t take the course of treatment your fingers will gradually turn to pretzel sticks and crumble away, your brain will become a giant chicken heart and eat Philadelphia, your best friend will never speak to you again, and you will have a Migraine every day forever.”
I don’t know about you, but I’d go for the treatment. And I don’t even want to be a blond!
Okay, I’m being extreme. I hope I didn’t lose you there in all my silliness; there really is a point. It is rarely given to us to know whether we are making the right choice, before, during, or after. We have to weigh our options, but then we just have to choose.
Before I had my first child I fell and herniated a disk in my low back, causing two years of back pain. Then I had a difficult labor with an erratic pattern of contractions, wearing me out without making progress. After 18 hours of labor, I chose to use pitocin, a synthetic hormone, to stimulate the labor, and the pitocin made the contractions strong and painful enough that I felt I needed anesthesia. I had to choose between taking pain-killers and having an epidural (where anesthetic would be injected into the dura, or sack, around my spine). With an epidural there was a chance that my disk problem could become worse, even to the point of permanent back pain. With pain-killers, if I ended up with a cesarian section, I would need general anesthesia. The choice was to be awake for my daughter’s birth and risk disabling back pain, or to risk being knocked out for her birth with no back complications. I chose the epidural. I did have a cesarian; I was awake; and I did not develop any back problems from it.
My husband and I will never forget when I was lying in the birthing chair, pitocin-induced contractions sending me into ever higher spikes of pain and exertion, trying to make a choice in the panting moments between. We were 31 years old, and we felt like we became adults in that moment. If I had ended up with disabling back pain, I don’t know if I would have said it was the right choice. To be awake and hold Rachel in the moment after she came into the world was a joy I did not want to miss. That was what I chose. But who can say if it was the right choice?
The choice I made recently was to start on Migraine preventive medication. I spent at least 6 months making that choice. It was a choice I was considering for at least 4 years. Sometimes a choice needs to stew on the back burner of our minds. In that 6 months I:
• Found a doctor I could trust (which took several tries and months of waiting for appointments);
• Did a lot of on-line research, and read about other’s experiences with preventives;
• Recommitted to my meditation and relaxation program;
• Tried magnesium and B2 supplements;
• Tracked my Migraine numbers; and
• Talked about the decision with my friends on and off line, my husband, my family.
Eventually, the choice just felt clear.
I will be returning to this subject of choosing in several more posts in the near future – if you’ve read all the way down here I’ve kept you too long already! What I’ll leave you with today is to say that those times when you must make that life-changing decision right now are rare. We usually have some time to make our choices. Use that time. Let things simmer on the back burner. Let your subconscious mind do its job. Will you make the right choice? Nobody knows. But you can make the choice with much less anxiety in the meantime.
– Megan Oltman
Pretzel sticks image coutesy of Windell Oskay; image of window at Mesa Verde is by me to illustrate being between a rock and a hard place – Mesa Verde is all rocks & hard places. And amazing.
Tags: childbirth, chronic illness, Indiana Jones, making choices, Migraine disease, Migraine treatment, pitocin
Posted in Managing, Medicine, Silliness | Comments (7)
Highlights from the American Headache Society Annual Conference
July 1st, 2008
 Last week the American Headache Society held its 50th annual conference in Boston. You may have read other news of the proceedings and the many new discoveries, inventions, understandings, and treatment options that were presented at the conference. Lead expert Teri Robert of My Migraine Connection and Migraine blogger Eileen of My Life with Migraine attended the conference and will be posting a lot of information in the weeks to come. If I may relay some tidbits second-hand, I was inspired to hear of their experiences in a collegial atmosphere where a number of dedicated medical professionals and advocates are working and sharing ideas to help bring us relief from this life-stealing disease. I wish I could have gone along, but first things first. I need to get my own migraines under better control before attending conferences, which have always tended to trigger me. Though I suppose there might be no better place to be with a migraine!
Last week the American Headache Society held its 50th annual conference in Boston. You may have read other news of the proceedings and the many new discoveries, inventions, understandings, and treatment options that were presented at the conference. Lead expert Teri Robert of My Migraine Connection and Migraine blogger Eileen of My Life with Migraine attended the conference and will be posting a lot of information in the weeks to come. If I may relay some tidbits second-hand, I was inspired to hear of their experiences in a collegial atmosphere where a number of dedicated medical professionals and advocates are working and sharing ideas to help bring us relief from this life-stealing disease. I wish I could have gone along, but first things first. I need to get my own migraines under better control before attending conferences, which have always tended to trigger me. Though I suppose there might be no better place to be with a migraine!
The conference will provide material for many posts, both here and all around the Migraine blogosphere. I’m going to share a couple of highlights that I am particularly interested in, and we’ll touch on more of the new information as I have a chance to digest it.
One new device which looks promising is the transcranial magnetic stimulation, or TMS, device. Tested for use by those suffering from Migraine with Aura, the TMS device is held at the base of the skull at the first sign of aura (visual and sensory disturbances experienced by about 20% of migraineurs). You push a button to deliver two short magnetic field pulses to the brain. Apparently these pulses scramble and abort the abnormal electrical activity which takes place in the brain during a Migraine attack. The basic black and white model looks good for this raven-haired lady; maybe they’ll come out with some more colors soon! But seriously, this is a great alternative, since everyone can’t use triptans, and even if you can, triptans knock you out of action for a while.
 New research was presented about Why Pain Becomes Chronic. New understandings of how pain becomes chronic can help headache specialists develop new therapies which can help sufferers with Chronic Daily Headache. One of the new understandings involves the role of glial cells in the brain, which agitate neurons, increasing pain signals to the brain. Use of opiates appears to activate glial cells, so can contribute to the development of chronic pain. Research was also presented indicating that expectation of pain affects its severity, that in the case of chronic pain, the nervous system “over-reacts” but that this overreaction is physiological, not psychological. A very important distinction – biological changes have been observed in the nerves themselves. In other words, the pain is “all in our heads,” in physiologic structures in the brain, not “all in our heads” in any psychosomatic sense. I must say I feel vindicated – read my post It’s All in your Head on the difference between what’s in our heads physiologically and the old psychosomatic accusation we are so often subjected to.
New research was presented about Why Pain Becomes Chronic. New understandings of how pain becomes chronic can help headache specialists develop new therapies which can help sufferers with Chronic Daily Headache. One of the new understandings involves the role of glial cells in the brain, which agitate neurons, increasing pain signals to the brain. Use of opiates appears to activate glial cells, so can contribute to the development of chronic pain. Research was also presented indicating that expectation of pain affects its severity, that in the case of chronic pain, the nervous system “over-reacts” but that this overreaction is physiological, not psychological. A very important distinction – biological changes have been observed in the nerves themselves. In other words, the pain is “all in our heads,” in physiologic structures in the brain, not “all in our heads” in any psychosomatic sense. I must say I feel vindicated – read my post It’s All in your Head on the difference between what’s in our heads physiologically and the old psychosomatic accusation we are so often subjected to.
Yet another piece I am particularly interested in deals with Migraine in women and the role of hormones and the menstrual cycle. More on that when I know more!
Overall, the good news is, there are good people out there looking out for us, working hard to find ways to treat this disease.
– Megan Oltman
Neurons image courtesy of Rebecca Radcliff.
Tags: American Headache Society, Chronic Daily Headache, chronic pain, glial cells, Migraine treatment, Migraine wih Aura, transcranial magnetic stimulation
Posted in Advocacy, Medicine, Science | Comments (4)
Managing my Migraines: Recent Success
June 25th, 2008
 All my hidden superstition comes out and I hesitate to say this for fear of jinxing myself, but I have only had one very mild Migraine in the past 19 days. It is too soon to tell if this is a trend or a fluke. It’s quite a contrast to the last 6 months though, when I’ve had an average of 5 Migraines per month and my Migraines have generally lasted 36 hours. I promise not to be embarrassed if this trend doesn’t continue. I believe I am doing a lot of right stuff – just sometimes we need even more right stuff to add to our toolkits.
All my hidden superstition comes out and I hesitate to say this for fear of jinxing myself, but I have only had one very mild Migraine in the past 19 days. It is too soon to tell if this is a trend or a fluke. It’s quite a contrast to the last 6 months though, when I’ve had an average of 5 Migraines per month and my Migraines have generally lasted 36 hours. I promise not to be embarrassed if this trend doesn’t continue. I believe I am doing a lot of right stuff – just sometimes we need even more right stuff to add to our toolkits.
I have yet to try preventive medications; I missed my long-awaited headache specialist appointment when I was sick with bronchitis. But I will give you my current regimen, and list the things that I think are making a difference. Please note that this is my list; the same factors might not work for you.
- 400 mg of Magnesium (see studies done by USDA linking magnesium deficiency and migraine)
- 200 mg of B2 (riboflavin)
- a high potency multi-vitamin
- 60 mg Armour Thyroid*
- an iodine supplement*
- 3000 mg phosphorylated serine per day, 1000 mg each at lunch, dinner and bedtime*
- 10 mg DHEA*
- the Wiley Protocol – bio-mimetic hormone replacement therapy
- not drinking caffeinated beverages more than 2 -3 times per week – and the ones I drink are mild!
- 30 – 45 minutes aerobic exercise daily
- sleeping 8 hours per night
- daily meditation
- basing my work schedule on the idea that I have about 30 productive hours in me per week, and not trying to do more than that!
- taking frequent breaks throughout the day and gardening or doing housework
- napping if I need to
- switching overhead lights in the house back from CFLs to incandescents
- banning my son’s stinky cologne from the house
- Summer – long days, warmth
I have Migraine disease, early stage chronic fatigue syndrome (CFS), low thyroid and, I believe, seasonal affective disorder. I also have allergies, and frequent, sometimes chronic, sinus infections, and am very prone to catching whatever illnesses are around to catch. The factors that I marked with an asterix (*) above are not there to prevent Migraine; they are there to balance my hormones, strengthen my adrenal glands, and manage my CFS. All the research shows that CFS and low thyroid are co-morbid conditions with Migraine – they occur at the same time, without a causal relationship. I can only speak to my own experience, but when I am fatigued, and I push myself beyond my limits, I often get a Migraine. Low thyroid also contributes to my fatigue, which contributes to my Migraine frequency. Unless someone can prove to me otherwise, I will maintain that taking care of my thyroid and CFS also takes care of my Migraines.
I began the Wiley Protocol about a year ago to address menopausal symptoms. The Wiley Protocol replaces a woman’s hormones with the identical hormones her body makes (rather than the synthetic hormones found in traditional HRT), and doses them in the way that mimics her natural cycle when she is young. It is not specifically designed to combat Migraine, but for those of us whose Migraines increased in peri-menopause, it makes sense that returning to a younger hormonal state would help! I found initially that while my Migraine frequency didn’t improve, the severity went way down. My doctor started me on an adjusted dose of the hormones about 3 weeks ago, with estrogen levels raised slightly in the beginning of my cycle and lowered slightly later on. Since that’s the same time period where I’ve been having so few Migraines, I can only guess it’s helping.
I am usually healthier in the warm weather months, and sluggish and illness-prone over the Winter. I feel like I come alive again in the Spring. Short of moving far south, I think I will have to get a light-box for next Winter to address this.
The CFLs are funny for me. They are on a list of things that I “just don’t like” – and haven’t liked most of my life (baking in the hot sun, strong men’s colognes, crowded rooms full of noisy people, fluorescent lights). Lo and behold, these things that I never liked are actually triggers for me. When I began blogging about CFLs a month or two ago it occurred to me to get them out of my own house and see what happened. My husband had started replacing incandescents with CFLs in our overhead lights about six months ago. My Migraine frequency went way up when? About six months ago! Coincidence? We’ve been taking them out again and… fewer Migraines?
A conclusion here? As you all know who deal with this disease, there are many factors involved. If you are one of those people who only has to avoid one trigger, or take one herb, or use one particular drug, to eliminate Migraines, then God bless you! You have my undying jealousy! If you are one of those complicated cases who have to manage multiple triggers and multiple treatments, I know how tired you are of managing it all. I just want to hold out some hope – that the detective work is worth doing, and can make a difference. Keep on trying!
– Megan Oltman
Managing Migraines one day at a time.
Crossed fingers image courtesy of Meisje van de Sliterij.
Tags: chronic fatigue syndrome, magnesium, Migraine treatment, Migraine triggers, the Wiley Protocol, vitamin B2
Posted in Managing, Medicine | Comments (8)
Migraine? Where do I Start?
June 20th, 2008
Do you have migraines? Severe, disabling head pain, sometimes accompanied by flashing lights and other visual disturbances, usually accompanied by nausea, light and sound sensitivity? If you do, you know how Migraine disease can impact your life.
- The pain can strike at any time. When it comes, it throbs and pounds on one or both sides of your skull.
- People around you may not understand. Most people have headaches,
but only 12% of us have Migraine disease. You may feel guilty and
question yourself – are you making too big a deal out of this? - Your migraines may seriously impact your ability to perform on your job.
You may risk job loss from frequent unpredictable absences or inability to perform at top productivity. - You may be tired of all the wasted hours spent in darkened rooms. You may despair at your inability to keep the basic routines in your life moving forward.
- Maybe you have not sought medical help. Maybe you thought you should be able to handle it on your own. Maybe you sought medical help but didn’t get it, because your doctor doesn’t understand migraine, or because you were turned away at the emergency room as a drug-seeker.
- You may be overwhelmed by all there is to manage, even with medical help – treatments, lifestyle changes, remembering all your meds and supplements at the right times, tracking your migraine triggers, recognizing patterns.
And while dealing with all of this, you struggle to remember that you are more than just your migraines.
You are not just a patient, or a chronically ill person. You are a unique human being with things to contribute, people who love you, talents and strengths.
If you fit these characteristics, the first thing I have to tell you is, there is hope. While there is no cure for Migraine disease, there are many proven strategies and treatments that can reduce your migraines
and enable you to take back your life.
Many of us struggle along for years, either with or without the diagnosis of “Migraine,” taking pain killers and coping with the migraines when they come, and then something happens. The pain gets worse, the attacks get more frequent, the symptoms change; suddenly what we always did to cope doesn’t work any more. We need answers. We pick up a book, talk to a doctor, search the internet. And we discover there is a lot of information, a lot of misinformation, and loads of people trying to sell us “cures!”
I wrote the free e-course “The Six Keys to Manage Your Migraines and Take Back your Life” to help people in that situation – people who are trying to get the information and support they need to cope with, manage, and recover from debilitating migraines. I wrote it to help people start down the path to managing their migraines and taking back their lives.
In the The Six Keys to Manage Your Migraines and Take Back your Life we discuss:
- What Migraine disease is: the more you know about Migraine, the more power you will have over it.
- How to get good medical support.
- How to recognize your triggers and your early warning system for Migraine.
- The value of a good Migraine calendar and diary.
- Cultivating support systems of people and routines to help you manage your life.
- Using relaxation to calm your nervous system and reduce your migraines.

I would love to have you use the course as a resource for yourself as you work on managing your migraine disease. If you’d like to register for The Six Keys to Manage Your Migraines and Take Back your Life just fill out the box at the upper left corner of this page. The e-course will be delivered to you by email every two days over approximately two weeks. As you receive each lesson, take some time to think about how it applies in your life, and follow the action steps included in each lesson. I will be available by email for help and feedback as you work your way through the course.
For over ten years I have worked to help my clients live healthier, more productive lives. I am certified as a life and business coach; I am also a migraineur. I have succeeded in reducing my migraine frequency and severity by over 50% through a combination of medication and lifestyle approaches. I have run my own business for fifteen years while managing Migraine and several other chronic illnesses. I am committed to helping people live healthy and productive lives, creating a thriving world we all want
to live in. For those of us with Migraine disease, that means more than relief from pain – it also means living the best lives we can, using our talents, and knowing our strengths.
This is the game I love to play. You can play it with me!
– Megan Oltman
Please come out to play!
Cave exit photo courtesy of David Wilmot; Smoo cave waterfall photo courtesy of Subflux
Tags: Migraine disease, Migraine treatment
Posted in Managing, Tips & Techniques | Comments (3)
Botox for Migraine Treatment – News?
March 10th, 2008
In today’s London Daily Mail, reporter
The FDA is not advising doctors to stop prescribing the drug, but
they are conducting a safety review and say the reactions may be due to
overdosing. However, they are warning patients that they should receive
immediate medical attention if they have worsening or unexpected
difficulty in swallowing or talking, trouble breathing or muscle
weakness following any injection of Botox.
The dangers appear to be acknowledged in the Botox labeling. Migraine Blog reported on February 8, 2008, that:
The Warnings sections of the labeling for both botulinum toxin products
note that important systemic adverse effects, including severe
difficulty swallowing and difficulty breathing have occurred in
patients with neuromuscular disorders after local injection of typical
doses of botulinum toxin. FDA now has evidence that similar,
potentially life-threatening systemic toxicity from the use of
botulinum toxin products can also result after local injection in
patients with other underlying conditions such as those with cerebral
palsy associated limb spasticity. Systemic toxicity has been reported
in children, several of whom required feeding tubes and/or ventilation
(breathing) support.
Migraineurs please read the research, and follow up with your doctor if you have any concerns.
– Megan Oltman
hypodermic image courtesy of happysnappr/Adrian Clark
Tags: Botox, Migraine treatment, US FDA
Posted in Medicine | Comments (2)
That disclaimer thing...
Remember: nothing we do here is medical advice or treatment or is a substitute for medical advice or treatment. Get competent medical advice to learn more about your migraines, possible treatments and risks.
What's New on Migraine Support Group Coaching |
Recent Comments
- on Calling all Redheaded Migraineurs
- on No, You’re not Crazy, You just Have Migraines
- on No, You’re not Crazy, You just Have Migraines
